The world’s Largest Sharp Brain Virtual Experts Marketplace Just a click Away
Levels Tought:
Elementary,Middle School,High School,College,University,PHD
| Teaching Since: | Apr 2017 |
| Last Sign in: | 327 Weeks Ago, 4 Days Ago |
| Questions Answered: | 12843 |
| Tutorials Posted: | 12834 |
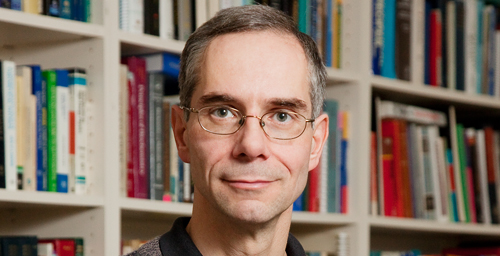
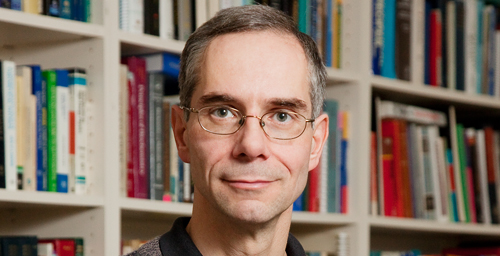
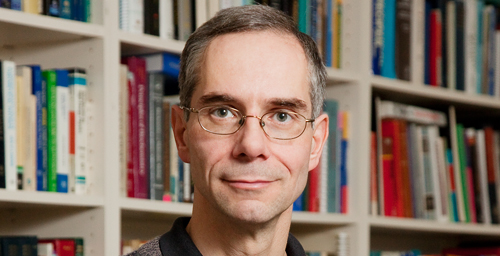
MBA, Ph.D in Management
Harvard university
Feb-1997 - Aug-2003
Professor
Strayer University
Jan-2007 - Present
В Jack Green (J.G.) is a 55 year old white male who lives in the city. He is widowed, with 2 grown children. He lives in a small second-floor apartment, and is employed as a used car salesman. He works long hours, usually 10-12 hours a day, and 6 days a week. Neither of his children live near enough to visit often, but they call every week or two to see how he is doing. They used to call more often, but since their mother died, J.G. just isnГўt interested in talking. He has become somewhat withdrawn and irritable at times, so they are not a close family like they used to be.
В В В В J.G. has frequent complaints of ГўindigestionГў, but he has never seen a health care provider for advice or treatment. He uses a lot of over the counter antacid pills, which really do not give him much relief. In fact, he has not seen a doctor since his wife passed away 2 years ago. When she was alive, she made sure that J.G. got regular check-ups, and monitored his blood pressure. She also saw to it that he got enough rest, ate well, and took care of himself. He was in much better health then.
В В В В Now that he lives alone, J.G. does not pay attention to his diet or any other self-care activities.В He eats fast food most of the time. He often says, ГўWhy cook for one person?Гў Currently his weight and blood pressure are out of control. He sleeps only 3-4 hours per night, and sleep is often interrupted, either by restlessness or by having to get up and urinate often due to an enlarged prostate. He has also started smoking again, about 1 pack per day, and says that smoking is the only thing that calms his ГўnervesГў although he admits he is much more short of breath now that he is smoking again, often to the point of having to stop and rest to catch his breath frequently even when walking a short distance or up the stairs to his apartment. He also has a terrible cough in the morning when he first awakens.
В В В В One day at work, right after lunch, J.G. seemed to be in more discomfort than usual with his ГўindigestionГў. He had chest pain and became diaphoretic. A co-worker called 911 and J.G. was taken to the local Emergency Room for evaluation. On arrival at the E.R. his blood pressure was 186/102. Mild rhonchi were heard throughout all lung fields. No cardiac murmur was heard. He had 2+ pitting edema in both lower extremities. His face was very flushed, restless, and he was slightly hyperventilating.
В В В В He feared he was having a heart attack, but fortunately he was not. Lab tests and EKG were negative, but revealed elevated cholesterol and triglyceride levels. Chest x-ray showed mild cardiac enlargement and lungs were normal. He was stabilized, kept for observation for several hours, and then released.
В
On discharge, the medical diagnoses were as follows:
В В В В 1. Uncontrolled hypertension
В В В В 2. Cardiomegaly
В В В В 3. Obesity
В В В В 4. Gastro-esophageal reflux (GERD)
В В В В 5. Hyperlipidemia
В В В В 6. Possible Depression
В В В В В В В В В В В В В В В В В В В В В В В В В В В В В В
His discharge orders were as follows:
В В В В 1. Lisinopril 20mg po qd (for blood pressure)
В В В В 2. Nexium 40mg po qd (for relief of GERD)
В В В В 3. Simvastatin 20mg po qd (for elevated lipids)
В В В В 4. Low Na / Low fat diet.
В В В В 5. Smoking cessation classes
В В В В 6. Follow up with primary care provider within 2 weeks for physical exam andВ В В В В В В В В В В В В В В В В В В В В В
В В В В В В В В depression screening.
В
В В В В You are the nurse working in the primary care office. Since it has been so long since J.G. has had any type of health care, a complete health history and physical exam is indicated at the next scheduled visit.
В В В В When J.G. arrives for his exam, he denies current indigestion symptoms but states he is having trouble avoiding fast foods because ГўItГўs just too much work to cook and eat alone.Гў He has not been able to cut back on his smoking yet, either, and reports that he still smokes at least 1 pack per day, and occasionally maybe more since discharge from the hospital because the experience made him Гўvery nervous.Гў On the day of his physical exam, J.G.Гўs weight is 346 pounds, height 6Гў1Гў, which calculates to a BMI of 45.6 indicating obesity. He is fairly quiet during the assessment, answers questions politely and appropriately, but makes little eye contact. He is oriented x 3, speech clear and not pressured, and thoughts are logical.
В В В В As you begin taking his health history, J.G. admits that he is ГўscaredГў and upset that his health has gotten so out of control. You recognize that he is now more aware of his health issues and perhaps ready to make some positive changes. You also see an openness toward learning Гў and decide to take advantage of these Гўteachable momentsГў as you offer health education and health promotion.
-----------